Cardiac biomarker testing is estimated to occur in nearly 30 million emergency department visits nationwide each year in the United States. The American College of Cardiology/European Society of Cardiology indicate that cardiac troponin is the biomarker of choice owing to its nearly absolute myocardial tissue specificity and high clinical sensitivity for myocardial injury. Multiple academic medical centers have implemented interventions to eliminate the routine ordering of creatine kinase–myocardial band tests, with published patient safety outcomes data; however, creatine kinase–myocardial band testing is still ordered in many hospitals and emergency departments. Eliminating a simple laboratory test that provides no incremental value to patient care can lead to millions of health care dollars saved without adversely affecting patient care quality, and in this case potentially improving patient care.
Introduction
Acute coronary syndrome (ACS) is one of the leading causes of mortality in the United States. Since the 2000 American College of Cardiology (ACC)/European Society of Cardiology (ESC) redefinition of acute myocardial infarction (AMI), which was revised into the 2007 and 2012 Universal Definition of AMI, cardiac troponin (cTn) has been the biomarker of choice owing to its nearly absolute myocardial tissue specificity and high clinical sensitivity for myocardial injury.1,2 Cardiac troponin is preferred by both clinical (ACC/ESC/American Heart Association [AHA])3- 5 and biochemical (National Academy of Clinical Biochemistry)6,7 guideline groups, for similar reasons. In the most recent universal definition of AMI, creatine kinase-myocardial band (CK-MB) is described as an alternative to be used only if cTn is not available.2 The 2014 AHA/ACC guidelines conclude that CK-MB provides no additional value for diagnosing AMI (class III, level of evidence A).5
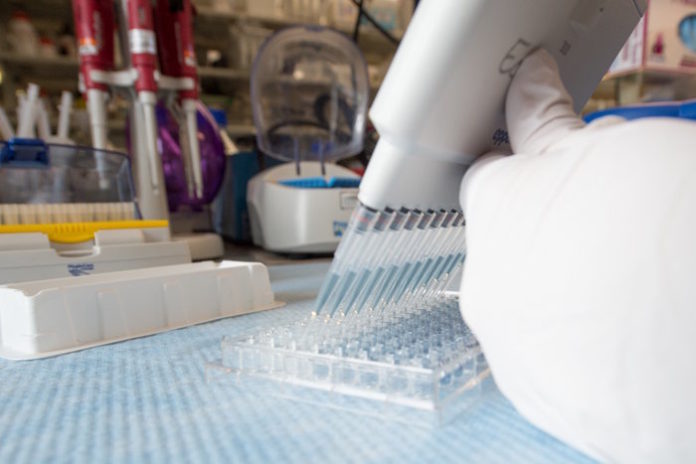
The ideal biomarker test for the diagnosis of AMI should be highly sensitive and specific, rapidly obtained and analyzed, and lead to treatment decisions that provide high value, in terms of clinical benefit relative to cost.8 The importance of this goal stems from the sheer number of patients receiving cardiac biomarker testing and the resulting contribution to health care expenditure in the United States each year. In 2010, Makam and Nguyen9 showed via the National Hospital Ambulatory Medical Care Survey (n = 44 448 emergency department [ED] visits) that cardiac biomarker testing (both cTn and CK-MB) occurred in 16.9% of all visits to the ED. The authors extrapolated this to represent 28.6 million ED visits nationwide. Considering Medicare’s 2016 Clinical Diagnostic Laboratory Fee Schedule10 (national payment amounts for cTn and CK-MB of $13.40 and $15.73, respectively), approximately $416 million is spent on cardiac biomarker testing annually. Not included in these estimates are additional unnecessary expenditure and potential harm associated with subsequent noninvasive and invasive testing that may result from false-positive results.
Once the cornerstone of AMI diagnosis, CK-MB has not yet been eliminated from practice despite considerable evidence supporting cTn as the preferred biomarker.8,11 Data published after distribution of the ACC/ESC/AHA3- 5 recommendations show the these clinical practice guidelines have not succeeded in refining practice. Specifically, CK-MB is still used in many US clinical pathology laboratories and US EDs.12,13 Based on the College of American Pathologists proficiency survey in 2013, 1558 of 1995 national US laboratories (77%) still use CK-MB.12 In 2009, Parker and Suter13 surveyed 98 ED physician leaders in 21 academic and 77 community EDs regarding the use of cardiac biomarkers and found that 77% (76 of 98) still use CK-MB. Collinson et al14 found that of the nearly 40% of North American and European laboratories (n = 533) offering CK-MB testing in 2006, 25% continued to offer the test even after the national guidelines discussed above recommended against its use. Cappelletti et al15 added to the findings by Collinson et al14 by adding data from Italy (n = 126 laboratories) that showed 20.2% of laboratories continue to use CK-MB.
This retention of CK-MB has been attributed to clinicians’ reluctance to rely on cTn in certain clinical situations, as well as clinician familiarity.8,11 In 2010, a study coauthored by 7 large academic medical centers labeled CK-MB as 1 of 10 tests that no longer provide value,16 and a growing number of medical centers have abandoned use of CK-MB.8 With the goal of advancing high value practice, as defined by the ACC, ESC, AHA3- 5 and National Academy of Clinical Biochemistry, this implementation guideline is designed to assist institutions in eliminating unnecessary CK-MB testing.
Evidence-Based Guidelines: Troponin and CK-MB Tests
Numerous studies have compared CK-MB and cTn with respect to their diagnostic precision related to the initial diagnosis of AMI, the assessment of reinfarction, and prognosis after major cardiovascular events. Cardiac troponin has been shown to be highly sensitive for AMI (99.2%)17 and to be more specific than CK-MB (lower false-positive rate) owing to its exclusivity in cardiac myocytes (vs CK-MB, which may be elevated with skeletal muscle damage).16- 19 Hawkins et al20 calculated a specificity of cTn testing as high as 92% compared with 40% for CK-MB. Lin et al21 observed that among patients with suspected AMI who also had negative cTn results, approximately 10% of patients had abnormally high CK-MB.22 Similarly, Antman et al23 evaluated cardiac biomarker levels in patients with ACS symptoms and found that 238 of 948 patients (25%) initially classified as having unstable angina owing to normal CK-MB tests actually had elevated cTn levels. Thus, the use of CK-MB may potentially misclassify individuals with ACS by mistakenly diagnosing unstable angina in some patients with true myocardial infarction.
In patients with chronic renal disease, the diagnosis of ACS can be challenging, as cTn levels may be chronically elevated. However, CK-MB has been shown to provide no incremental value over cTn in the diagnosis of ACS in patients with chronic renal disease.24,25 In fact, CK-MB levels are often elevated in patients on dialysis in the absence of ACS signs and/or symptoms.25
In terms of time to diagnosis, both CK-MB and troponin are equally rapid in ACS diagnosis,8 but with more sensitive assays, cTn rises much more rapidly.26- 28 In addition to its superior sensitivity and specificity, cTn yields stronger prognostic information. In patients with ACS, the CRUSADE investigators (n = 29 357)29 showed that elevated cTn is associated with in-hospital mortality, regardless of CK-MB levels. However, when CK-MB levels are elevated in the presence of a normal cTn, in-hospital mortality is comparable to CK-MB levels and cTn both being negative.29- 31 Most important, those with elevated CK-MB values but normal cTn levels do not manifest an adverse prognosis.29- 31
Despite a longstanding, commonly held physician belief that CK-MB is more useful than cTn for detecting reinfarction, no study has shown that CK-MB levels are superior to cTn in this regard.32,33 Indeed, most data confirm that cTn provides far better estimates because it is less impacted by changes in the amount of marker released with reperfusion.34 Single values correlate closely with infarct size as determined by cardiac magnetic resonance imaging.35 Apple et al36 showed that both biomarker levels rise similarly with reinfarction. The most recent ACC/AHA/ESC guidelines support the use of cTn over CK-MB for diagnosing reinfarction.3- 5
Most patients with ACS are treated with either surgical or percutaneous revascularization.37,38 The use of CK-MB or cTn following percutaneous coronary intervention (PCI) is controversial, as there is no current consensus regarding the definition, prognosis, and subsequent treatment of periprocedural myocardial infarction diagnosed by cardiac biomarker elevation alone. Some groups have suggested that CK-MB is superior to cTn in terms of detecting periprocedural myocardial infarction,38 while others have argued that post-PCI cardiac biomarkers are not useful because prognosis is related to the pre-PCI cTn value, and when that is taken into account, post-PCI myocardial injury is not an important clinical end point.39 Even if clinicians decide to assess cardiac biomarkers in this setting, post-PCI cTn and CK-MB values provide equally accurate prognostic information.39 Because this guideline is focused on cardiac biomarker use in routine ACS diagnosis, rather than cardiac biomarker use following PCI, we defer further discussion and/or recommendation with respect to this ongoing clinical controversy.
Another potential area of controversy concerns the appropriate use of cTn in clinical practice.40 The major strength of using cTn—its specificity for cardiac injury—is also a potential shortcoming, because cTn detects myocardial injury irrespective of the specific cause. Consequently, many noncardiac conditions associated with secondary myocardial injury, such as pulmonary embolus, severe anemia, and severe hypotension from any cause, are associated with abnormal cTn. Wilson et al40 reported a high prevalence of elevated cTn in a large group of hospitalized patients due to noncardiac conditions and has suggested that this may represent an example of overuse of cTn. Another group has reported a small series of patients in which the quantity of troponins ordered per patient exceeded guideline recommendations.41 We acknowledge that the real-world use of cTn, with respect to appropriate clinical indication and quantity over time, deserves further study and quality improvement initiatives designed to refine usage.
Finally, Saenger et al8 have observed that concomitant use of CK-MB and cTn is often confusing for physicians, and they are aware of situations in which such confusion has negatively affected patient care. An example of a potentially confusing clinical situation is when a patient is admitted with possible symptoms of ACS and is found to have an abnormally elevated CK-MB levels in the setting of sequentially normal troponin levels. Although normal sequential troponin values exclude the diagnosis of acute myocardial injury—and are associated with a favorable short-term prognosis regardless of the CK-MB levels—some physicians might erroneously conclude that the patient has suffered acute myocardial injury due to CK-MB elevation. Others might wonder if there is another condition (ie, skeletal muscle breakdown) responsible for the CK-MB elevation and might erroneously devalue the importance of the patient’s symptoms and electrocardiogram in making the diagnosis of ACS.42 We would argue that elimination of routine CK-MB ordering is not only high value because it offers no benefit and results in considerable cost but also because elimination of CK-MB may reduce physician confusion, improve understanding of the proper use of cTn, and consequently reduce potential patient harm.
Safety and Quality Outcomes Data: Eliminating CK-MB Testing
Multiple academic medical centers have implemented interventions to eliminate the routine ordering of CK-MB and measured associated cost savings and impact on patient safety (Table).12,43- 46 Larochelle et al44 recorded data on patients with suspected ACS (n = 60 494 patients preintervention; n = 24 341 patients postintervention) over a period of 43 months (31 months preintervention; 12 months postintervention). They initially developed an institutional guideline in collaboration with cardiologists to specify appropriate ordering of cardiac biomarkers for the diagnosis of AMI. The guideline advised practitioners to order cTn alone, without CK-MB. The authors then implemented multiple interventions, including educational sessions for internal medicine and ED physicians, dissemination of pocket-sized quick reference cards with the recommended ordering algorithm, and removal of CK-MB from ACS routine order sets within the computerized provider order entry (CPOE) system. A Best Practice Advisory (BPA) was created in the CPOE system using the institutional guideline to alert physicians who attempted to order CK-MB. Physicians could, if desired, order CK-MB manually. By 12 months postintervention, the estimated number of CK-MB tests per patient was 0, representing an absolute change of −0.96 CK-MB tests per patient (95% CI, −1.00 to −0.92). The authors estimated a 95% reduction in CK-MB tests, translating to $720 000 in annual savings.
Similarly, Baron et al43 removed CK-MB from routine order sets and implemented a BPA into their CPOE system without additional educational sessions. After only 2 months postimplementation, they noted an 87% decrease in CK-MB orders. In addition, they noted fewer orders after searches and fewer searches for CK-MB over this time, arguing for a long-term educational benefit for the BPA. Multiple other groups, including Mayo Clinic, simply removed CK-MB from routine order sets and found 80.0% to 99.8% reductions in CK-MB orders with significant cost savings and without negative impact on patient care or missed AMI diagnoses.8,12,43- 46
Implementation Blueprint: Eliminating CK-MB Testing
With clear evidence to support elimination of CK-MB from clinical care for the diagnosis of ACS and based on experience eliminating CK-MB at our respective institutions, we devised a blueprint for other institutions to use in enacting quality improvement initiatives. The methodology and theory of the blueprint and quality improvement initiative are based on the US Health Resources and Services Administration strategies for developing and implementing a quality improvement initiative, with a focus on education, action, and measurement of results.47 The leader of each institution should assess applicability of this blueprint based on the CK-MB ordering frequency at their respective institution.
- Design and implement a hospital-wide educational campaign.
- Prior to implementation, it is important for health care leaders to establish sufficient organizational readiness for change, specifically in conjunction with these stakeholders, whose ordering practices will be affected by such changes. Tools to measure readiness for change have been previously studied and may be used.48,49
- Collaborate with physician representatives from the departments of cardiology, internal medicine, and emergency medicine. Frontline physicians in these departments order the majority of cardiac biomarkers within most health care institutions and are the primary stakeholders in the current system of care for ACS patients.
- Academic institutions must engage the house staff as members of the quality improvement team for an effective initiative.
- Collaborate with secondary stakeholders, such as pathology and/or laboratory staff, to acquire insight and advice on these changes.
- Inform physicians that CK-MB adds to the health care system financial burden without adding value to patient care.
- Present the evidence supporting elimination of CK-MB and exclusive use of cTn to diagnose AMI, identify reinfarction, and estimate infarct size. Education may be provided through various venues, including lectures, pocket cards (Figure 2), online modules, social media demonstrations, and simulations.44
- Partner with information technology and/or laboratory medicine staff to remove CK-MB from standardized ACS routine order sets. Doing this simple step alone has been shown to significantly reduce CK-MB ordering (Table).8,12,45,46
- Partner with information technology and/or laboratory medicine staff to create and integrate a best practice alert into the CPOE to appear when clinicians order CK-MB, such as:
- According to national guidelines, troponin is the preferred biomarker for detecting myocardial injury; CK-MB is only appropriate if troponin testing is unavailable. Figure 1 provides an example.43,44
- Measure data preintervention and postintervention (efficacy points).
- Number of cTn and CK-MB tests ordered, including stratification by department and patient setting (ED, inpatient, medicine vs nonmedicine units, ICU vs non-ICU).
- Incidence, missed diagnoses, and mortality of AMI to ensure patient safety.
- Review cases where CK-MB is still ordered to determine if it provides value.
- If necessary, track usage by physician to develop performance feedback profiles.
- Calculate reduction in charges to patients and health plans, as well as any decrease in hospital costs.
Though seemingly straightforward to articulate, we acknowledge that significant barriers to implementation exist, and in this case the biggest hurdle has been convincing physicians who have ordered CK-MB for years to change their practice. Successful deimplementation of CK-MB requires leadership support, education, and reassurance that diagnostic efficacy will not be compromised. Other challenges relate to manpower as well as modifications and data collection from the electronic medical record. To optimize manpower, academic centers can engage house staff because this will also ensure longstanding change. Again, leadership commitment to allocating information technology resources for data collection and clinical decision support tools is critical.
Conclusions
Creatine kinase–myocardial band testing provides no incremental value to patient care, and its elimination can lead to millions of health care dollars saved without adversely affecting patient care. This is backed by both strong evidence-based guidelines and experiences from multiple institutions. The blueprint presented here should be carefully considered by health care leaders and clinicians as the first step to finally putting the CK-MB laboratory test to rest.
Acknowledgements: This article is the first collaborative scholarly activity produced by faculty in the High Value Practice Academic Alliance (HVPAA). The HVPAA organization includes faculty from dx.doi.org/…161/CIRCULATIONAHA.107.187397more than 80 academic medical centers collaborating on quality improvement, research, and education related to high-value healthcare.
References
- Department of Radiology and Radiological Sciences, Johns Hopkins Hospital, Baltimore, Maryland
- Division of Cardiology, Department of Medicine, Mayo Clinic, Rochester, Minnesota
- Division of Cardiology, Department of Medicine, Johns Hopkins Bayview Medical Center, Baltimore, Maryland
Source: jamanetwork.com








[…] Infobioquimica […]
Comments are closed.